EDITORIAL
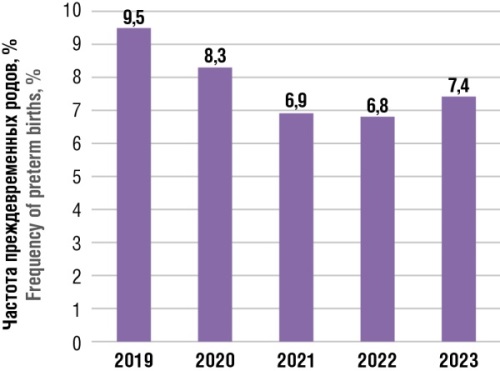
This journal issue presents studies devoted to actual questions of women's health, including thrombophilia impact on pregnancy, determination of biological age in the reproductive period, and the relationship between placental pathology and thrombophilic disorders. Innovative approaches to diagnostics and treatment are considered, such as plasmapheresis in antiphospholipid syndrome, organ-preserving strategies in placenta accreta spectrum, and prospects for passive fetal monitoring using machine learning. Immune-mediated thrombotic complications, including vaccine-induced thrombotic and heparin-induced thrombocytopenia, are highlighted. Clinical cases of rare pathologies are presented, such as lipodermatosclerosis in pregnant women, complete androgen insensitivity syndrome, and laparoscopic cerclage for cervical insufficiency. The final material is dedicated to Robert Edwards historical role in the development of in vitro fertilization.
ОRIGINAL ARTICLES
What is already known about this subject?
► Preeclampsia (РЕ) is defined as a new-onset hypertension and proteinuria or other target organ damage occurring at age later than 20 weeks of gestation. It occurs in 4–6 % of pregnancies and accounts for over 70,000 maternal deaths and 500,000 fetal/neonatal deaths annually worldwide.
► Depending on the onset, a distinction is made between early-onset and late-onset РЕ occurring before 34 weeks and at least 34 weeks of gestational age, respectively.
► РЕ is based on a multifactorial pathogenesis; however, its etiology, especially in the context of early-onset and late-onset РЕ, is not fully understood.
What are the new findings?
► The epidemiology and pattern of thrombophilic defects differ between pregnant women with early-onset or ''placental'' РЕ (before 34 weeks) and late-onset or ''maternal'' РЕ (after 34 weeks).
► Pregnancy considered as a hypercoagulable state, however, even small changes in coagulation and fibrinolysis can contribute to adverse pregnancy outcomes such as РЕ.
How might it impact on clinical practice in the foreseeable future?
► Adequate analysis of genetic thrombophilia and fibrinolytic system polymorphisms, as well as testing for antiphospholipid antibodies (aPL), homocysteine and metalloproteinase ADAMTS-13 blood content may be useful in identifying women at РЕ risk.
► Timely PE pathogenetic prevention includes administration of low doses of acetylsalicylic acid starting from 13 weeks of pregnancy. Perhaps, detection of thrombophilia can change the treatment tactics by applying therapy from earlier pregnancy terms, which will prevent development of such a formidable pregnancy complication.
Aim: to study a pattern of genetic and acquired thrombophilia in pregnant women with severe early-onset (eoPЕ) and severe lateonset (loPЕ) preeclampsia (PE).
Materials and Methods. A retrospective cohort study was conducted from January 2022 to May 2024. A total of 109 pregnant women were examined: group 1 – 45 women with eoPЕ (< 34 weeks of pregnancy), group 2 – 24 women with loPЕ (≥ 34 weeks of pregnancy), group 3 (control) – 40 women with physiologically uncomplicated pregnancy. All pregnant women were examined for lupus anticoagulant (LA) and antiphospholipid antibodies (aPL). The screening test for aPL included the quantitation of IgG/IgM antibodies against cardiolipin, phosphatidylserine, phosphatidylinositol, phosphatidic acid, and β2-glycoprotein 1 in serum or plasma using an enzyme immunoassay. Genetic thrombophilia, homocysteine, and ADAMTS-13 metalloproteinase (a disintegrin and metalloproteinase with thrombospondin type 1 motif, member 13) levels were also determined.
Results. Pregnant women with severe PE more often had genetic forms of thrombophilia (mutations in factor (F) V Leiden gene, prothrombin G20210A, and Thr165Met) and a deficiency of natural anticoagulants (antithrombin and protein S) compared to pregnant women in control group. Women in eoPE vs. loPE group were more often found to carry genetic polymorphisms in the plasminogen activator inhibitor-1 (PAI-1) and fibrinogen genes. Also, in the group of pregnant women with eoPE, the circulation of aPL, ADAMTS-13 inhibitor, and elevated homocysteine levels were more common. Pregnant women with loPE were older and more often suffered from hypertension, diabetes mellitus, and excess body weight. No significant differences between eoPЕ and loPЕ groups were found while comparing prevalence of autoimmune diseases, thrombosis in familial history, mutations in FV Leiden gene (heterozygous form), FII prothrombin gene G20210A (homozygous form), FII prothrombin gene Thr165Met (heterozygous form), antithrombin III deficiency, protein S deficiency.
Conclusion. Precise causes underlying PE remain unknown, andwe are still far from understanding all the molecular, immunological, genetic, and environmental mechanisms that lead to the various clinical manifestations of placental syndromes including PE. However, the study results suggest that the presence of thrombophilic disorders, especially in the fibrinolytic system, and aPL circulation contribute to eoPE pathophysiology or progression.
What is already known about this subject?
► Biological age (BA) reflects body physiological state and does not always overlap with passport age, which is especially important in reproductive medicine.
► Existing methods for calculating BA are often based on limited data and do not take into account the features of reproductive age women, thereby underlying a need to develop new, more accurate methods.
► Oxidative stress affects health being related to diseases and can accelerate aging, emphasizing an importance of body antioxidant function.
What are the new findings?
► A new method for BА calculation is proposed for women aged 20–45, taking into account their physiological state and reproductive function.
► The proposed method for calculating BA includes the overall antioxidant status (OAS), which allows for a more accurate assessment of individual aging rates.
How might it impact on clinical practice in the foreseeable future?
► The implementation of the proposed model in reproductive medicine will increase effectiveness of women's health monitoring.
► Taking into account the OAS in clinical practice can lead to development of individualized approaches to disease treatment and prevention.
Introduction. Biological age (BA) reflects the characteristics of the morphological and physiological state of the human body at a specific period of its life.This concept is of particular importance in reproductive medicine, because actual age does not always correlate with the state of organs and systems.
Aim: to develop a method for calculating BA for women aged 20–45 years, considering their physiological state and reproductive function.
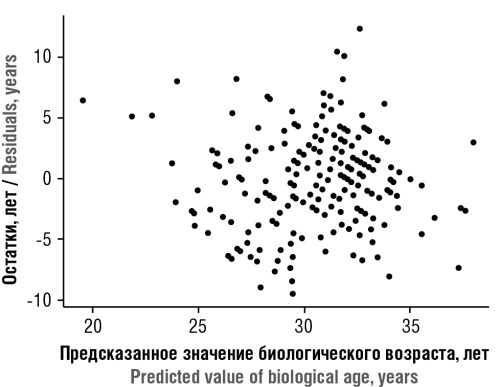
Materials and Methods. A single-stage non-randomized cohort study was conducted. To create the BA calculation model, a study was conducted with 100 healthy women aged 20–45 years. Seventy-eight parameters were analyzed, including anamnesis data, anthropometric parameters, data of general blood test, biochemical blood test, instrumental studies, assessment of overall antioxidant status (ОAS), from which the most informative variables were selected. The model was developed using multiple linear regression.
Results. The most informative indicators for calculating BA were: ОAS, static balance time (SBT), body mass index (BMI), and number of former pregnancies. The developed BA calculation formula demonstrated high accuracy, correlating with chronological age (correlation coefficient of 0.947).
Conclusion. The proposed BA calculation method is specifically designed for women of reproductive age and shows high accuracy and correlation with chronological age. The inclusion of antioxidant protection parameters, functional state indicators, and reproductive history makes the method versatile and applicable not only in reproductive medicine but also in general medical practice, obstetrics, gynecology, and other fields.
What is already known about this subject?
► Thrombophilia can contribute to uterine vascular thrombosis, which can alter blood supply to the placenta and lead to its abnormal development.
► Anomalies in the placenta location can be caused by an impaired placenta formation, which can occur due to placental vessel thrombosis.
► In the presence of thrombophilia, the risk of developing obstetric complications increases, especially in combination with placenta previa. This can lead to serious consequences such as fetal growth restriction (FGR), premature birth, and an higher likelihood of bleeding during and after childbirth.
What are the new findings?
► A high frequency of thrombophilia was found among patients with placenta previa, which highlights a relationship between genetic and acquired thrombophilia and placenta previa.
► Placenta previa is associated with increased FGR risk, detected by ultrasound fetometry. This is especially evident for recurrent placenta previa.
► The study shows that patients with placenta previa are more likely to develop uterine hypotension and atony, deep vein thrombosis.
How might it impact on clinical practice in the foreseeable future?
► Considering high frequency of thrombophilia among patients with placenta previa, preconception screening for thrombophilia in risk groups may reduce a risk for mother and child.
► It is necessary to develop a strategy for using anticoagulant therapy in such female cohort that may assist in reducing a risk of obstetric complications associated with thrombophilia and placenta previa.
► Detection of combined placental location anomalies and FGR may serve as an important prognostic marker for significant blood loss during delivery and other complications.
Aim: to test the hypothesis about a connection between genetic and acquired thrombophilia, as well as the characteristics of delivery in women with placental abnormalities.
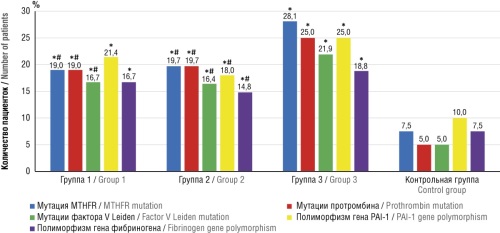
Materials and Methods. A prospective controlled cohort non-randomized interventional study assessing the characteristics of delivery and the presence of thrombophilia was conducted in 135 women with placental abnormalities. Pregnant women were divided into 3 groups: group 1 included 42 women with a history of placental abnormalities; group 2 – 61 pregnant women with placenta previa first discovered during ongoing pregnancy; group 3 – 32 women with recurrent placenta previa. The control group included 120 pregnant women who had a normal placenta position and no complicated obstetric history. All women had a clinically assessed course of pregnancy, underwent ultrasound, testing for congenital and/or acquired thrombophilia by detecting antiphospholipid antibodies (APA), identification of genetic forms of thrombophilia: mutations in the 5,10-methylenetetrahydrofolate reductase (MTHFR) gene, mutations in the prothrombin gene G20210A, factor V Leiden mutations, assessment of present fibrinogen and plasminogen activator inhibitor 1 gene polymorphism.
Results. Thrombophilia was found in a significant percentage of patients with placenta previa (74.81 %), and the majority – with the multigene form belonged to group 3. The combination of genetic thrombophilia and APA circulation was detected in 22.22 % of patients. Signs of fetal growth restriction (FGR) were identified in all study groups: 4 (9.52 %) in group 1, 6 (9.84 %) in group 3, 6 (18.75 %) in group 3 and in 6 (6.67 %) in control group. All patients in the study groups underwent delivery by cesarean section (CS) – in 31 patients it was premature at 35–37 weeks due to increased fetoplacental insufficiency and the development of fetal distress syndrome: in 10 (23.8 %) pregnant women of group 1, in 12 (19.7 %) of group 2, and in 9 (28.1 %) women from group 3. In 104 women, CS was performed at 37–38 weeks of gestation. In the group of women with recurrent placenta previa (group 3) the frequency of complications during delivery significantly differed from similar those in groups 1 and 2 (p < 0.05) and control group (p < 0.001): 13 (40.6 %) cases of uterine hypotension were identified, 6 (18.8 %) uterine atony cases and 5 (15.6 %) cases of placenta accreta, which required hysterectomy in 7 (21.9 %) patients. In 4 (12.5 %) cases, clinically significant signs of deep vein thrombosis (DVT) were detected.
Conclusion. The study results indicate a connection between placenta previa, genetic thrombophilia and emergence of complications during delivery. The need to adjust approaches to the management of pregnancy delivery by taking such risk factors into consideration was discovered.
What is already known about this subject?
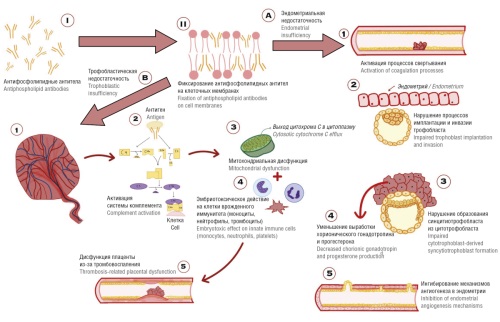
► Antiphospholipid syndrome (APS) is a disease associated with antiphospholipid antibodies (АРА) circulation, which lead to thromboinflammation and pregnancy complications: pre-
eclampsia, placental insufficiency, recurrent miscarriages, fetal growth restriction, ets.
► The complement system plays an important role in APS pathogenesis. Activation of the complement system promotes the release of proinflammatory and antiangiogenic mediators, which in turn alter placenta formation.
► The «gold standard» for APS treatment is the use of low-molecular-weight heparins and low doses of acetylsalicylic acid. Nevertheless, a paucity of evidence exists in the literature to evidence an efficacy of plasmapheresis (РР).
What are the new findings?
► A PP course during preconception preparation leads to a decrease in circulating APA level in patients with APS.
► In main group, 98.65 % of pregnancies resulted in childbirth suggesting that preconception care is an effective strategy for patients with APS.
How might it impact on clinical practice in the foreseeable future?
► The additional РР use during preconception care demonstrated a decline in circulating АРА titers and an higher likelihood for favorable pregnancy outcome.
Aim: to study plasmapheresis (PP) effect on antiphospholipid syndrome (APS) treatment during preconception preparation and pregnancy.
Materials and Methods. A single-center, prospective, randomized, uncontrolled study was conducted. A total of 137 women aged 22 to 32 years diagnosed with APS-related habitual miscarriage were examined. The patients were stratified as follows: main group consisted of 73 patients underwent a PF course (7 procedures at preconception preparation stage); comparison group – 64 patients not underwent efferent therapy. Antiphospholipid antibodies (APA) circulation was determined by solid-phase immunofluorescence. PР was performed using an intermittent technique. The laboratory study included assessing titers of lupus anticoagulant (LA), anti-cardiolipin antibodies (aCL), anti-β2-glycoprotein 1 antibodies (anti-β2-GP1) and anti-annexin V antibodies (anti-ANX). Antibody titers were measured before and after pregravid preparation.
Results. After PР, anti-β2-GР1 titers decreased by 66.6 % (p = 0.00001) in main group. In patients who underwent standard therapy without PР, no significant changes in circulation level of anti-β2-GР1 were noted. LA frequency in main and comparison group decreased by 57.3 % (p = 0.042) and 10.9 % (p = 0.69), respectively.
Conclusion. The frequency of detecting elevated AРA levels in women after a course of efferent therapy decreased significantly, whereas standard therapy showed no such effects. PР as part of complex therapy is more appropriate for achieving maximum effect.
What is already known about this subject?
► The method, based on assessing scattered light and its interaction with matter, creates a special “biochemical imprint”.
► Surface-enhanced Raman spectroscopy (SERS) is used not only in medicine, but also in other fields, such as biology, pharmacy, forensics, etc.
What are the new findings?
► A non-invasive method for diagnosing benign ovarian formations (OF) in pregnant women is presented.
How might it impact on clinical practice in the foreseeable future?
► SERS may be considered as a potential research method in pregnant women with ovarian neoplasms.
► SERS will reduce the frequency of OF over-diagnosing, and will also help to make right decision on OF removal during pregnancy.
Aim: to study the spectral characteristics of blood plasma in pregnant women with benign ovarian formations (OF).
Materials and Methods. A retrospective study conducted between 2021 and 2023 included 100 pregnant women aged 18 to 45 years. Two groups were identified: group 1 (main group) included 50 pregnant women with OF, group 2 (control group) included 50 pregnant women with normal pregnancy. Using the method of surface-enhanced Raman spectroscopy (SERS), we determined and assessed the spectral features typical to OF, which are necessary for differential diagnosis of this pregnancy-related pathology.
Results. Prominent inter-group differences in spectral intensities were revealed: OF was associated with significantly increased intensity of spectral peaks at 491 nm, 596 nm, 632 nm, 808 nm, 886 nm, 1132 nm and decreased intensity at the peaks of 725 nm and 1440 nm observed compared to control group. After OF removal, spectral pattern restored to near complete compliance with the spectral pattern observed in control group of pregnant women.
Conclusion. The isolated and analyzed spectral features demonstrated an opportunity of using SERS in diagnosing OF in pregnant women.
REVIEW ARTICLES
What is already known about this subject?
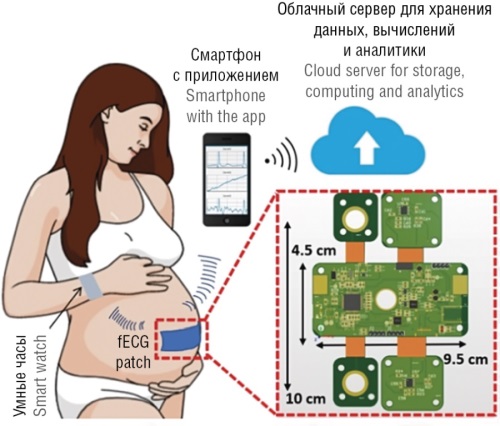
► Assessment of fetal functional state is an integral part of obstetric practice. Existing methods of prenatal diagnostics using sensors with active ultrasound radiation have a number of limitations: lack of prognostic value, impossible continuous long-term monitoring of fetal health indicators, insufficiently high diagnostic accuracy. It necessitates development of new technologies to assess fetal functional state allowing to overcome the above limitations.
► To date, developments in the field of creating wearable systems based on the use of passive sensors are underway. The introduction of such systems in the future will allow for long-term and continuous monitoring of fetal vital signs.
What are the new findings?
► The article provides an overview on innovative methods for long-term fetal monitoring using passive sensors, such as accelerometers and microphones. It describes systems integrating machine learning for data analysis, which enhances diagnostic accuracy and prognostic potential. The article also analyzes the advantages, limitations, and development prospects for such technologies.
How might it impact on clinical practice in the foreseeable future?
► The implementation of wearable fetal monitoring systems based on passive sensors will enable long-term and continuous fetal observation in home settings. This will allow for more accurate and timely detection of fetal distress, reducing the incidence of perinatal complications. Such technologies will expand monitoring accessibility and optimize the workflow of healthcare professionals.
Introduction. Prenatal diagnostics of fetal vital activity includes regular assessment of parameters such as heart rate (HR), motor activity and physiological state. Current methods of fetal monitoring based on using active ultrasound waves have a number of limitations: insufficiently high diagnostic sensitivity and specificity, lack of prognostic significance and impossible long-term use. These limitations necessitate a development of innovative technologies for assessing fetal functional state.
Aim: to summarize advanced global developments as an alternative to ultrasound systems for long-term fetal monitoring, allowing continuous real-time recording of fetal vital signs by using passive sensors and trend analysis with potentially high diagnostic and prognostic accuracy.
Materials and Methods. The review methodology included an analysis of publications released over the past 10 years, included based on relevance criteria. Publications were selected in accordance with the PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines. The following keywords in Russian and English were used for selection: "modern methods of prenatal diagnostics", "fetal monitoring", "assessment of fetus functional state", "passive sensors", "artificial intelligence", "machine learning". The search yielded 69 articles in the PubMed/MEDLINE database, 17,500 – in Google Scholar, 21 – in eLibrary, and 3,563 – in ResearchGate. Such articles were analyzed for relevance, relevance to the review topic, and availability of experimental data. Non-peer-reviewed publications and duplicates were also excluded from the reviewed materials. The most relevant 8 articles were included in the review, which describe promising methods of prenatal diagnostics based on the use of passive sensor experimental devices.
Results. The conducted literature analysis allowed to generalize the experimental achievements of current methods of prenatal diagnostics and demonstrated great promise for automated systems to assess fetal vital signs, including monitoring fetal HR, motor activity and general functional state. However, it was found that none of the described systems achieves 100 % accuracy of the results corresponding to fetal cardiotocography and ultrasound examination data. Most experimental systems remain wired, which limits their use for fetal monitoring. Promising passive monitoring systems are based on using accelerometers, microphones and other sensors to assess fetal functional state. A key component of such technologies is the use of artificial intelligence for signal processing and interpreting, which increases the accuracy and monitoring information content. The main problem is generation of effective data processing algorithms for their accurate and unambiguous interpretation. All the technologies under consideration are still experimental, and further work is required to improve the algorithms and integrate various types of sensors to ensure comprehensive analysis.
Conclusion. It is noteworthy that technologies employing passive sensors for continuous and long-term monitoring of fetal vital signs, in conjunction with machine learning algorithms for data analysis and interpretation are of particular interest. The use of wearable devices, based on passive sensors such as accelerometers and digital microphones, has the potential to enhance prenatal diagnostics, ensuring both enhanced safety and the early detection of pregnancy complications and fetal conditions.
What is already known about this subject?
► Currently, the main therapeutic approach for placenta accreta spectrum (PAS) is peripartal hysterectomy characterized by a high rate of postoperative complications and inability to plan pregnancy.
► Obstetricians and gynecologists have been increasingly turning to alternative uterus-preserving PAS interventions, which also reduce a risk of complications, providing women with possibility of pregnancy in the future.
► Uterus-preserving methods of PAS treatment are presented as uterus resection-reconstruction and delayed interval hysterectomy.
What are the new findings?
► Organ-preserving treatment requires longer timeframe, but lowers a risk of complications and improves a woman's quality of life in the future. Peripartal hysterectomy is effective in the short term, but is related to a higher risk of complications.
► Organ-preserving PAS treatment allows to avoid serious surgery and preserve a possibility of pregnancy in the future, however, prolonged postpartum monitoring can be painful and inconvenient. It is important that a pregnant woman participates in decision-making, even if a single strategy is preferred for medical or logistics reasons.
► Fertility rate in PAS individuals is unchanged after organ-preserving treatment. Study data show that 83–89 % PAS patients with mean 17.3 months post-treatment were able to become pregnant. All pregnancies preserved after the first trimester of pregnancy ended with the birth of a healthy child.
How might it impact on clinical practice in the foreseeable future?
► Organ-preserving PAS treatment allows to preserve female fertility, which is extremely important in the current demographic situation.
► Organ-preserving treatment may require longer timeframe to achieve a desired result, but it can lower a risk of complications and improve a woman's quality of life in the long term. Along with this, peripartal hysterectomy may be more effective in the short term, but it is related to a higher risk of complications.
► A possibility of preserving uterus with placenta in situ and subsequent organ-preserving management allows for an individual treatment approach, taking into account the desires and needs of each patient.
Introduction. Placenta accreta spectrum (PAS) is the preferred term approved by most international organizations that refers to the range of pathologic adherence of the placenta. PAS is a serious problem with incidence rate of 1/272 in-labor women. Today, peripartal hysterectomy is considered as the generally accepted global practice for PAS management, however, this approach is related to high level of maternal mortality and the impossibility of pregnancy in the future.
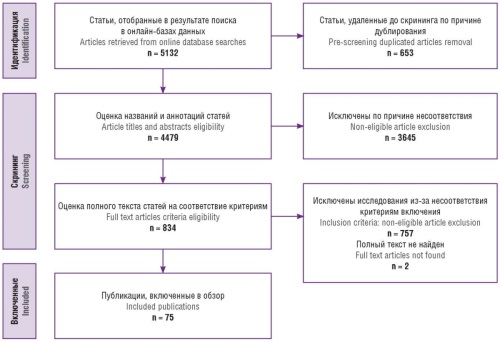
Aim: to analyze publications on the available methods for PAS diagnostics and management by highlighting organ-preserving treatment including assessment of relevant risks and benefits compared with other methods as well as prospects for patients.
Materials and Methods. Research papers were searched for in the databases eLibrary, PubMed and Google Scholar released until August 2024. The following search queries were used: "placenta accreta spectrum", "PAS", "PAS and organ-preserving treatment", "PAS and peripartum hysterectomy", "PAS and organ-preserving management". The selection of articles was carried out in accordance with the recommendations of PRISMA initiative that allowed to analyze 75 publications included in the review.
Results. Organ-preserving PAS treatment is a reasonable alternative to peripartal hysterectomy, because it provides better results with lower risk to maternal health. It is worth noting that each of these methods has own unique features. For instance, organpreserving treatment may last longer to achieve a desired result, but at the same time it can reduce a risk of complications and improve a woman's quality of life in the long term. Along with this, peripartal hysterectomy may be more effective in the short term, but it is associated with a higher risk of complications.
Conclusion. A doctor should provide a woman with all the necessary information about the risks and benefits of each method, as well as help a woman make an informed decision based on her individual needs and preferences. Organ-preserving PAS treatment contributing to preserve fertility offers a better quality of life with lower risk to maternal health. Ultimately, a choice between peripartal hysterectomy and organ-preserving treatment depends on a specific situation as well as woman's state of health.
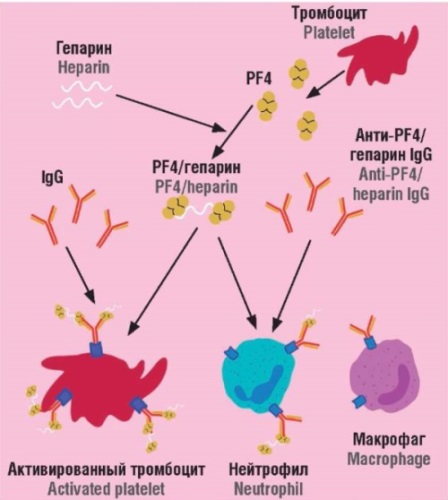
What is already known about this subject?
► Vaccine-induced immune thrombotic thrombocytopenia (VITT) is a rare but severe immunological reaction associated with adenoviral vector-based COVID-19 vaccines.
► VITT is a potentially life-threatening complication characterized by the development of thromboses, predominantly in atypical locations such as the cerebral venous sinuses and mesenteric vessels in combination with severe thrombocytopenia.
► Heparin-induced thrombocytopenia (HIT) and VITT share a common pathophysiological mechanism involving production of anti-platelet factor 4 (PF4) antibodies and the subsequent development of thrombotic complications.
What are the new findings?
► The article provides a description of the pathogenesis of PF4-related platelet disorders including various HIT forms (classical, autoimmune, and spontaneous), as well as the VITT molecular mechanisms including spontaneous, non-vaccine-associated cases.
► Emerging evidence suggests that VITT may not be exclusive
to SARS-CoV-2 vaccines.
► The article outlines a diagnostic algorithm for the rapid identification of PF4-related platelet disorders; key differences in the pathogenesis and management strategies for VITT and HIT are reviewed.
How might it impact on clinical practice in the foreseeable future?
► Understanding VITT epidemiology and mechanisms is essential for guiding future research and ensuring vaccine safety.
► Optimizing therapeutic strategies, including the use of novel anticoagulants and immunosuppressive approaches, is a priority task to reduce mortality and improve outcomes in patients with VITT and HIT.
Aim: to carry out a comparative analysis of the pathogenesis, clinical manifestations, diagnostic criteria as well as therapeutic strategies of vaccine-induced thrombotic thrombocytopenia (VITТ) and heparin-induced thrombocytopenia (HIT), two rare but potentially life-threatening conditions associated with antibody-dependent platelet activation.
Materials and Methods. Current data on the pathogenesis, epidemiology, clinical presentation, diagnosis, and treatment of VITТ and HIT have been reviewed including an analysis of existing diagnostic scoring systems, laboratory tests, and therapeutic approaches. The study is based on the data obtained from systematic reviews, clinical studies, and up-to-date clinical guidelines.
Results. VITТ and HIT share a common pathophysiological mechanism involving the production of antibodies against platelet factor 4 (PF4) and subsequently developing thrombotic complications. However, a key difference lies in the triggers of the immune response: HIT is induced by heparin exposure, whereas VITТ develops following the administration of adenoviral vector vaccines against SARS-CoV-2. HIT is primarily characterized by venous thrombosis, while VITТ predominantly manifests with atypical thromboses, including cerebral venous sinus thrombosis. Both conditions require immediate medical intervention; however, HIT management involves discontinuation of heparin and the initiation of using alternative anticoagulants, whereas VITТ treatment requires administration of intravenous immunoglobulins and anticoagulants, including heparin-based agents.
Conclusion. Despite their rarity, VITТ and HIT pose significant health risks to patients. Modern diagnostic methods, including the 4Тs scoring system and serological testing, facilitate the timely identification of HIT, whereas VITТ diagnostics remains a complex challenge and requires further standardization. Optimizing therapeutic strategies, including the use of novel anticoagulants and immunosuppressive approaches, is a priority task to reduce mortality and improve patient outcomes.
CLINICAL CASES
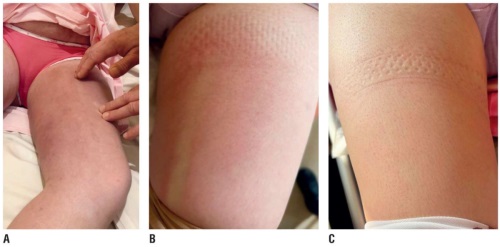
Pregnancy and childbirth in women with varicose vein disease (VVD) are typically associated with a high risk of developing thrombotic, obstetric and fetal complications. Lipodermatosclerosis (LDS) is one of the less common complications related to chronic venous insufficiency (CVI). This article presents a clinical case where LDS developed during late-stage pregnancy (35–36 weeks) as a complication of pre-existing VVD, which is noteworthy due to the rarity of such condition that demonstrates relevant diagnostic challenges particularly during pregnancy. Enhancing the effectiveness of a multidisciplinary approach is essential for diagnosing rare VVD complications in pregnant women.
What is already known about this subject?
► Cervical insufficiency (CI) is one of the leading causes of pregnancy loss and is diagnosed in a substantial percentage of women with habitual miscarriage.
► Transvaginal cerclage is the most commonly used surgical method for correcting CI but is ineffective in case of cervical anatomical changes such as scarring or conization. Transabdominal cerclage (TAC) is considered an alternative for such complex cases and can be performed via laparotomy or laparoscopy, showing high success rates for prolonging pregnancy.
What are the new findings?
► This article describes a successful case of in-pregnancy laparoscopic TAC underlining its effectiveness in cases of severe cervical pathology. It presents a TAC clinical case using the Cervix-set tape at 13 weeks of gestational age demonstrating successful pregnancy continuation and birth of a healthy baby. The article emphasizes the advantages of laparoscopic TAC as a minimally invasive method that lowers surgical risks and improves chances of successful delivery in complex clinical cases.
How might it impact on clinical practice in the foreseeable future?
► The use of laparoscopic TAC could become a more widely accepted approach for treating CI in patients with severe cervical anatomical alterations, increasing the chances of successful pregnancy continuation. The minimally invasive nature of the laparoscopic procedure promotes faster recovery and lowers a risk of postoperative complications, making it a preferred option in complex clinical cases.
► The successful clinical case and literature review may encourage clinicians to consider broader use of this technique in specialized medical centers. In the long term, laparoscopic TAC could reduce the incidence of preterm births and perinatal losses in CI patients, improving overall reproductive outcomes.
Miscarriage remains one of the most pressing challenges in modern obstetric practice, markedly impacting birth rates and women’s health. One of the manageable miscarriage causes is presented by cervical insufficiency (CI) occurring in 0.2–2.0 % of all pregnant women and in 15.5–42.7 % of those with habitual miscarriage. Both conservative and surgical treatments, such as the use of obstetric pessaries or cerclage, are applied to prevent CI-related preterm birth. Transvaginal cerclage remains the most common procedure for CI correction. However, in certain situations, transvaginal cerclage may be inapplicable or ineffective due to prior cervical scarring, conization, or other anatomical alterations. In such cases, transabdominal cerclage (TAC) can be considered as an alternative. TAC, either performed via laparotomy or laparoscopy, has demonstrated successful pregnancy outcomes in 81–89 % of cases. This article provides a brief literature review on CI surgical treatment and presents a clinical case of successful pregnancy after laparoscopic TAC. The patient, with a history of severe cervical pathology and multiple pregnancy losses, underwent a laparoscopic TAC at 13 weeks and 3 days of gestational age using the Cervix-set tape. The pregnancy was carried to term, and a healthy baby was delivered via planned cesarean section at gestational age of 38 weeks. Thus, laparoscopic TAC is an effective alternative for patients with complex cervical anatomy requiring more advanced surgical intervention. This procedure achieves high success rates for prolonging pregnancy and ensuring favorable outcomes while minimizing risks for both mother and child.
What is already known about this subject?
► Alteration of androgen gene causes androgen insensitivity syndrome (AIS). Alteration results in jeopardized androgen signaling with 46,XY karyotype and infertility.
► Prevalence rate of 20,000–100,000 among live birth and classified as complete, mild and partial AIS.
► Generally, gonadectomy followed by hormonal replacement therapy is given during puberty.
What are the new findings?
► Reported an early case of AIS misdiagnosed as inguinal hernia by 16 years old.
► Peripheral cultural confirmed 46,XY karyotype rejecting Mayer–Rokitansky syndrome and confirmed AIS.
► Bilateral testicular gonads with atrophic testes and Leydig cells hyperplasia with 46,XY phenotype were detected. Mental distress and suicide attempt was observed after diagnosis.
How might it impact on clinical practice in the foreseeable future?
► Family history and symptoms history from primary amenorrhea to cyclic abdominal pain or urinary symptoms.
► Importance of сlinical investigation to assess axillary and pubic hair, breasts development.
► Bilateral swollen groin with external genitalia of females. Importance of pelvic sonogram, karyotype to confirm the absence of uterus and ovarian follicle tissue.
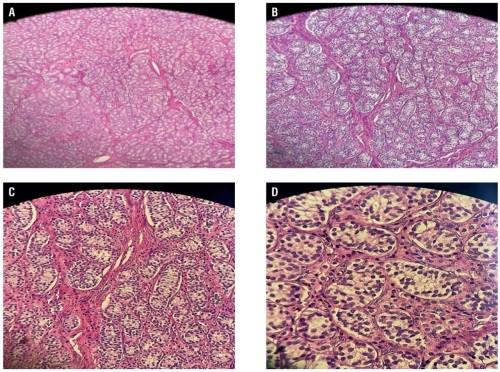
Complete androgen insensitivity syndrome (CAIS) is a rare X-linked sexual development condition typified by 46,XY karyotype, presence of external female genitalia along with intra-abdominal testes in labia majora or inguinal ring region. This syndrome results from alterations in the androgen receptor (AR) gene leading to primary amenorrhea and uterine agenesis (Müllerian agenesis) in adolescent teens or two-sided labial/inguinal hernia with testes in children around prepubertal age. Our paper reports a case of CAIS in a 16-year-old woman with no menarche and 46,XY karyotyping. Gonadectomy results showed hyperplasia of Leydig cells. The current research encompasses the case report and the available knowledge to date on the understanding, diagnosis, treatment, and management of CAIS.
FROM HISTORY
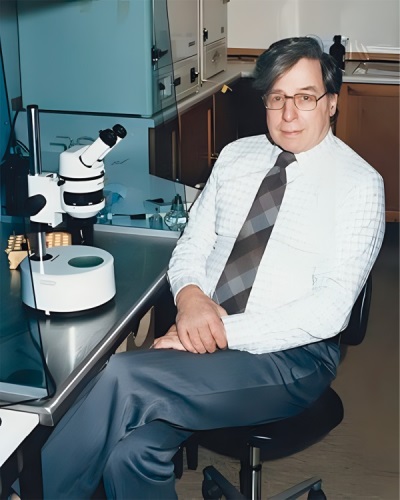
Here, we discuss the historical aspects of the life and scientific work of the British scientist Robert Geoffrey Edwards, who made a significant contribution to the development of reproductive medicine and genetics. Having begun with studying mouse physiology, together with colleagues he succeeded in proposing in vitro fertilization technique, which in 1978 led to the birth of Louise Brown, the world's first "test-tube baby". In 2010, Dr. Edwards was awarded the Nobel Prize in Physiology or Medicine for the development of human in vitro fertilization.
ANNIVERSARY

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
ISSN 2500-3194 (Online)